Leaky Gut: Potential Causes and Resolutions
What is leaky gut and what we can do to mitigate it?
👋 Hey there! My name is Summer. And I would really love to talk to you about something that I had been struggling with for many years. Why? Because if you are struggling with this too, then maybe this could be helpful for you in your journey to healing. My goal with this is to present you with all of the information that I have gathered over the years through my own experience and through my own research and share that information in the hopes that it could help to guide you in the right direction.
I have been managing leaky gut and autoimmune issues for the past 13 years. To be quite honest, it has probably been much longer than that. But the symptoms really began to show up intensely around that time. Just a few months after I had my first child, I began to experience really uncomfortable gut symptoms, along with some pretty severe skin rashes. It seemed to come out of nowhere and I was desperate for answers.
My skin was covered from the tips of my fingers up to my elbows in bright red skin overlayed with a silvery and flakey rash. I also had little pustules pop up in the palms of my hands and in between my fingers that were filled with fluid and were painful. And the itch I experienced was so intense I felt like I wanted to scratch down to the bone. And for whatever reason, the symptoms seemed to be at their worst during the night. More so in the very early hours of the morning between 1-3 am.
I was consuming ungodly amounts of Benadryl and using gobs and gobs of hydrocortisone cream just for some temporary relief. And at one point I even had to slather both of my hands and arms with antibacterial cream and wrap them with bandages for close to 2 weeks, along with taking a round of oral antibiotics, because my skin was cracking so badly that it had become infected.
Throughout the years I have had other symptoms show up as well like face and ear flushing, my entire face and neck swelling, my scalp becoming flaky and itchy, chemical sensitivities, food sensitivities, joint pain and stiffness, heart palpitations, hypertension, anxiety, candida overgrowth, and all kinds of stomach issues, leaky gut being one of them.
In my early twenties I also experienced about a year of some really severe brain fog. I was unable to focus. I could not think straight to save my life. Many times, even thinking at all was a challenge. And I was constantly forgetting things. Even in conversation with people I would often lose my thoughts and be stuck in a fog of nothingness. At one point I even forgot what my own name was for a few minutes. It was absolutely horrible. I don’t think people truly understand just how debilitating brain fog can be unless you have experienced it yourself.
Needless to say, with everything I was dealing with, I knew that I had to find answers. I questioned all sorts of potentials, like eczema, psoriasis, arthritis, lupus, Lyme disease, and Hashimoto’s disease. It felt like my body was breaking down. I was clouded with confusion, and I needed to understand what was happening to me and why. And so, my journey began.
I started paying visits to all sorts of specialists. I went to a general practitioner, an internist, an immunologist, an endocrinologist, a cardiologist, an allergist, and a dermatologist. And guess what? Noone could give me any answers. Not a single doctor that I saw could give me any solid leads as to why this was happening to me. The closest I came was the dermatologist.
When I first went to see her, she told me that she thought I had eczema, same thing that the immunologist told me. But even with that “diagnosis,” I still was not given any answers as to why or what to do. The dermatologist decided to do a skin biopsy on my hand. And when the results came back, she told me that I had psoriasis. And in fact, she suspected that I was dealing with both eczema and psoriasis. Her resolve? To put me on medication.
I will say that at least this doctor had the curtesy to tell me that the medication she was recommending had a side effect of potentially causing cancer. But I had already submitted myself to the answer of “no” before she had even told me that. I wanted to try to go about this in a natural way. Deep down I knew that there was more to the story. Deep down I knew that I could heal this on my own. And I was right. It has taken me many years to get to the point I’m at now. And there are some things I am still working to improve. After all, good health really is more of a moving journey than a destination.
But I hope that with me sharing this with you, it could help to save you from many years of struggle and grief. I will tell you that I do not have much in the way of qualifications. Shortly after this all began, after I had seen how the medical system was failing me, I decided that I wanted to become a Registered Dietitian so that I could go on to help people through the means of diet and lifestyle choices.
I had at that point discovered information about candida and leaky gut, and I started to make changes to my diet and lifestyle based around the information I was finding. I was seeing the impact that good diet and certain herbal supplements was having on my situation, and I knew that food could be a healing medicine.
This encounter with downward spiraling health sparked a passion in me. But unfortunately, while I was only 3 classes away from attaining my AS degree, life decided that it had other plans for me. Perhaps one day I will make it back to that endeavor. But for now, I will say that I am a Licensed Massage Therapist in the state of Texas who is speaking on this topic from true life experience. And I am a woman who has a very deep passion for health and a whole-body approach to healing.
So whatever information you find here that you think could be useful, I encourage you to go out and continue your own research and find whatever validation you need. And a little disclaimer, if you are currently working with a health care provider, make sure that you are speaking to them about things before jumping into any drastic changes.
The first part of this is going to be about the potential causes. We are going to look into the scientific biological functions of the systems involved to get a better understanding. The second part of this is going to be dedicated to the aspect of healing, or the “how,” by understanding and using the information from the “why.”
Let’s dig in!
Part One: The Why 🧠
What is leaky gut? 🤷♀️
Leaky gut, also known as increased intestinal permeability, refers to a condition in which the lining of the small intestine becomes damaged, allowing undigested food particles, toxins, microbes, and waste to leak through the intestinal wall and enter the bloodstream. Under normal conditions, the intestinal lining is selectively permeable—like a wise gatekeeper, allowing needed nutrients to pass through while keeping the harmful substances out. But with leaky gut, the tight junctions between intestinal cells become loose or compromised, creating microscopic gaps.
Image Source: Intestinal barrier: Tight junction
Image Source: Molecular Pathophysiology of Epithelial Barrier Dysfunction in Inflammatory Bowel Diseases
Your gut is not just seen as your stomach alone, but rather it is the entire system, or tube, that starts at the mouth and goes all the way through to the anus. And this system has some important roles to play:
It regulates fluid exchange and allows for the absorption of necessary vitamins and nutrients from your food into your bloodstream.
It keeps the unwanted bacteria and chemicals out of the bloodstream and keeps them confined within the tube so that they can be eliminated from the body.
It houses our much-needed microbiome, that when flourishing, allows us to keep our health regulated and radiant. Our microbiome supports healthy digestion, enhances immune function, positively impacts brain health and mood, helps to synthesize vitamins and proteins, protects against harmful pathogens, and regulates weight and blood sugar.
If your intestinal walls have “holes”, the bad stuff leaks into your bloodstream. This is not supposed to happen, and when it does it can lead to a range of health problems.
Why is leaky gut harmful to your health? 🤔
Over time your gut walls slowly become weakened. Typically, the first signs of you noticing something is off is from symptoms that are showing up in the digestive system. You may be experiencing things like:
Bloating
Gas
Diarrhea, constipation, or alternating bowel movements
Stomach pain
Heartburn or acid reflux
Mucus in the stool
Unfortunately, the symptoms do not stop there. Leaky gut issues normally extend to other areas of the body as well and include ongoing immune activation and persistent inflammation. You may also be experiencing things like:
Food sensitivities
Chemical sensitivities
Environmental sensitivities or allergies
Skin issues such as acne, eczema, or psoriasis
Fatigue or low energy
Headaches
Brain fog
Poor focus and concentration
Joint or muscle aches
Facial or body swelling
Autoimmune disorders
Mood changes
Nutrient deficiencies
Issues with weight or blood sugar
So, what causes leaky gut? 💡
While leaky gut is still a bit controversial in mainstream medicine, emerging research in genetics, gastroenterology and functional medicine is shedding light on the gut-brain-immune axis and how the integrity of the intestinal barrier is crucial to whole-body health.
While the desire may be to pinpoint a simple and specific cause (and believe me, I do understand that desire), the truth is that the cause of leaky gut could be multifactorial. This mishap in the system can be caused by anything that has the capacity to damage the intestinal lining and create inflammation. And it is likely a convergence of biological, emotional, and environmental stressors. And because of this it requires a multiheaded approach to heal.
What are some of the factors that could be causing damage?
Environmental sensitivities like mold, dust, pollen, etc.
Food sensitivities
High histamine foods and drinks
Dysregulated histamine genes
Mental and emotional stress
Physical stress from overexertion (like exercising too much)
Hormonal imbalances
Nutrient deficiencies
Gut microbes that are producing histamine, stimulating its release, or inhibiting other beneficial microbes from growing
Infections
Toxic overload (chemicals, heavy metals, etc.)
Elevated levels of zonulin
Many of these factors also cause a rise in histamine. And while histamine serves a very necessary purpose within the body, excess histamine causes disruption of those cell junctions in the gut lining which leads to intestinal permeability. Another big producer of elevated histamine is dysfunction with the DAO enzyme.
What is DAO? 🧬
DAO stands for Diamine Oxidase, a gene that encodes for an enzyme responsible for breaking down histamine, a compound involved in immune responses, digestion, and neurotransmission.
Histamine is vital, but like fire, it must be contained. It must be in a good balance. The image below this paragraph shows you the many uses of histamine as well as what is affected by histamine overload. The DAO enzyme is one of the primary regulators of histamine levels in the gut and bloodstream.
The HMNT gene enzyme also plays a role in breaking down histamine, especially in the brain, but DAO is primary in the gut. When the DAO gene is under-expressed, mutated, or the enzyme it produces is inhibited, histamine can accumulate—leading to a state known as histamine intolerance.
Image Source: Histamine and histamine intolerance
Here is a snapshot of my own DAO genes:
A genotype like this leads to a reduced function of the enzyme’s activity.
DAO breaks down exogenous histamine from food and bacteria in the gut. It works primarily in the small intestine, kidneys, prostate, colon and the placenta. And it provides protection from inflammatory overload, allergic-like reactions, and gut wall damage.
When the DAO gene is impaired, meaning there is a genetic mutation (SNP) or acquired deficiency in DAO function from lifestyle choices or environmental hazards, the result may be elevated histamine in the body, poor clearance of histamine from foods or gut microbes, and symptoms resembling allergies.
Symptoms of DAO Deficiency / Histamine Intolerance:
Headaches or migraines
Hives, rashes, or eczema
Itchy skin or itchy eyes
Nasal congestion
Nose bleeds
Heart palpitations, tachycardia or anxiety
Irritability or mood swings
Joint pain or stiffness
Digestive issues (bloating, diarrhea, cramping, heartburn)
PMS or irregular cycles
Insomnia or wakefulness at night
Flushing or overheating
Excessive sweating
Low blood pressure or dizziness
These can mirror some of the leaky gut symptoms because histamine overload further damages the intestinal lining, perpetuating a vicious loop.
But even if you do not have any single nucleotide polymorphisms (SNPs) of this gene, other factors that may contribute to low DAO enzyme activity could be intestinal damage from infections, celiac disease, IBS or IBD, nutrient deficiencies, certain medications like NSAIDs, antidepressants or antihistamines, or overconsumption of alcohol and histamine-rich or DAO-blocking foods such as aged cheeses, smoked meats or fish, wine, or fermented foods.
What role do hormones play in this? 🧩
The gut contains more hormone receptors than nearly any other tissue. It produces, activates, and detoxifies hormones. And the intestinal lining is responsive to fluctuations of hormones like estrogen, cortisol, insulin, and thyroid hormones. Thus, hormones can act as guardians or destroyers of gut integrity depending on their levels, rhythms, and interactions.
High or prolonged cortisol can disrupt tight junctions, suppress immune defense in the gut lining, decrease mucin production (your internal mucus shield), and increase inflammation, feeding the gut permeability loop.
Estrogen supports tight junction integrity, microbiome balance, and mucosal immunity. But when estrogen is too low, it can weaken the gut lining and provide lower immune resilience. When estrogen is too high, such as in estrogen dominance, that can increase gut inflammation and put you more at risk for something like candida overgrowth. Chronic estrogen dominance can also cause the release of pro-inflammatory cytokines and can stimulate mast cells, which releases excess histamine.
Progesterone soothes inflammation and enhances GABA, calming gut-brain reactivity. But when progesterone is too low that can increase stress reactivity and intestinal permeability.
The thyroid governs cellular turnover and immune signaling in the gut. Low thyroid (hypothyroidism) can lead to slow epithelial regeneration, reduced stomach acid, causing dysbiosis, and decreased gut motility. And Hashimoto’s Thyroiditis is frequently linked with leaky gut.
Low DHEA and low testosterone can increase gut inflammation and impair tissue regeneration and immune barrier function. And having balanced SHBG levels is important to help modulate free hormone activity in gut tissue.
Having unbalanced levels of hormones, especially for women, can be contributing to the problem and if we are going to tackle the issue head on, then getting your hormone levels tested and doing whatever is necessary for you or recommended by your physician to help regulate them should be a top priority.
I will say too that if you decide to have genetic testing done like I did, that can also help to shed a light on some of the potential issues when it comes to your hormones. It definitely did for me. I personally have genetic SNPs that affect my estrogen. And even though epigenetics can play a huge role in the way certain genes are expressed, I have been struggling with estrogen dominance and possibly thyroid hormone dysregulation. So, I have been on a bit of an aggressive and focused path to regulating my hormones over the past several years. I’ll show some of my SNPs just to give you an idea of some things to look for when it comes to this:
The DI01 gene deals with the conversion of T4 to T3. This indicates a possible decrease in that activity.
The CYP19A1 gene deals with the aromatase enzyme and the conversion of testosterone into estrogen. This indicates possible increase in aromatase activity which can lead to higher levels of estrogen.
The CYP1B1 genes deal with estrogen metabolites. This indicates possibly higher elevations of 4-OH estradiol, which is a more reactive form of estrogen and has been shown to be linked to breast cancer.
I personally have slower COMT activity. But the COMT V158M in particular is associated with metabolizing estrogen. Slower activity means reduction in estrogen metabolism.
Other genes to check for when it comes to hormones if this is something that interests you would be CYP17A1, HSD3B1 and HSD17B3, SHBG, AR, STAR and FSHR / LHCGR.
Now let’s take a look at number 12 on the list of causes, elevated levels of zonulin.
What is zonulin and what role does it play in leaky gut? 🧐
Zonulin is a protein that regulates the permeability of the tight junctions between cells of the intestinal lining. Think of these junctions like the clasps holding the fabric of the gut barrier together. When zonulin is released, these clasps loosen, allowing molecules to pass through the barrier.
This process is natural and necessary in moderation—it allows the body to sample antigens, regulate immune function, and respond to threats. But when zonulin is overexpressed, the intestinal lining becomes too permeable, leading to what we call leaky gut.
Elevations in zonulin have been associated with irritable bowel disease (IBD), celiac disease and irritable bowel syndrome (IBS). And people who deal with obesity, high blood pressure, high blood sugar, high triglycerides, high cholesterol, and autoimmunity have been shown to have elevated levels of zonulin.
Gluten, a protein found in wheat, barley, and rye, has also been shown to cause higher levels of zonulin by way of gliadin, a protein component of gluten. Gliadins are essential for giving bread the ability to rise properly during baking.
What Triggers Zonulin Release?
Gluten (particularly the gliadin component)
Bacterial overgrowth or infections
Environmental toxins
Chronic inflammation
Stress and trauma
Imbalanced microbiome
Now let’s take a look at the microbiome.
What is the impact of gut dysbiosis? 🦠
Gut dysbiosis refers to an imbalance or disruption in the composition, diversity, and function of the microorganisms that live your gastrointestinal tract—collectively known as the gut microbiome.
In a healthy state, the microbiome is a diverse and dynamic ecosystem where beneficial, neutral, and even some pathogenic microbes coexist in balance. When dysbiosis occurs, this balance is broken. Harmful microbes may overgrow, while beneficial ones diminish, leading to inflammation, malabsorption of nutrients, immune dysfunction, and even mental and emotional disturbances. Even beneficial gut bacteria can become dysbiotic when overgrown.
This dysbiosis is often caused by commonly prescribed medications such as antibiotics, PPIs, and NSAIDs. But other factors such as infections, gallbladder dysfunction, low stomach acid, diet, stress, and lifestyle factors may also contribute.
Types of Dysbiosis:
Loss of microbial diversity
→ Fewer species, less resilienceOvergrowth of pathogenic organisms
→ E.g., Candida, Clostridium difficile, Klebsiella, H. pylori, Salmonella, Giardia, CitrobacterDeficiency of beneficial microbes
→ Especially Lactobacillus, Bifidobacterium, Akkermansia, and others (though I will note here that while Lactobacillus strains have many benefits, many of them are actually histamine producing species, which can have negative effects on someone with leaky gut or histamine intolerance)Many pathogenic species are Lipopolysaccharide-producing species. LPS is an inflammatory bacterial endotoxin that can cause gut damage and leaky gut
Undergrowth of butyrate-producing species in the gut is also a problem. Butyrate is a short-chain fatty acid produced by certain colonic bacteria such as Faecalibacterium prausnitzii and Roseburia species. Short-chain fatty acids are metabolites produced when bacteria ferment soluble fibers. They are the food for certain bacteria and intestinal cells. Bifidobacteria produce a short-chain fatty acid called acetate that feeds butyrate-producing species. Butyrate provides energy to intestinal cells and protects the intestinal barrier against inflammation.
A few points on bile:
Bile acts like a natural soap, emulsifying dietary fats into microscopic droplets so enzymes like lipase can digest them efficiently. Without adequate bile, the body struggles to absorb Vitamins A, D, E, and K—the nutrients that fuel immune function, mood, hormonal health, and vision. Bile acids have natural antimicrobial properties, selectively suppressing the overgrowth of gram-negative bacteria and pathogens such as E. coli, Salmonella, and Clostridium difficile.
The composition of bile determines which microbes can thrive or perish. Certain beneficial bacteria like Lactobacillus and Bacteroides have evolved to tolerate bile and even use it to their advantage. Others are suppressed by it. Good bile production helps in preventing SIBO (Small Intestinal Bacterial Overgrowth), supports a diverse, healthy microbiome in the colon, and maintains a healthy balance in the ileum. Bile production and the gut microbiome are really working in a two-way relationship.
The gut microbiota also modifies bile acids into secondary bile acids, which have different effects. Some support metabolic health and insulin sensitivity, while others may become toxic or carcinogenic if dysbiosis is present. So, the state of the microbiome directly influences whether bile becomes healing or harmful, and vice versa. Ensuring you have good liver and gallbladder function, and a healthy and diverse microbiome is crucial to this process.
A fun little fact is that genetics plays a pivotal role in its production, composition, transport, and flow. If you are having any issues with your gallbladder or with bile, it could be related to your genes. There are several genes involved here, but one in particular that seems to have a somewhat common SNP, more so in women than in men, is the PEMT gene. (And interestingly, more women are dealing with autoimmune disorders than men).
PEMT stands for Phosphatidylethanolamine N-Methyltransferase. Its function is to convert phosphatidylethanolamine into phosphatidylcholine. And phosphatidylcholine is essential for keeping bile more fluid—not sludgy—and for building bile micelles that emulsify fat. Phosphatidylcholine makes up around 40% of the organic material in bile. And having an SNP in this gene could lead to:
Thick bile
Gallstone risk
Poor detox and fat absorption
Bile-driven leaky gut
Here is a snapshot of my own PEMT gene:
Another pretty telling sign for my situation.
Now let’s look at the toxic exposure aspect of this.
How do environmental toxins and chemicals affect gut health? ☢️
Our modern world is producing an environment laden with toxic overload. And while many of us do what we can to offset the impacts, it is still good to understand why there is a real need to do this.
There are so many toxins out there that contribute to our decline in health. We are constantly bombarded by these harmful substances; things like PFAs, VOCs, POPs, herbicides, pesticides, microplastics, heavy metals, mold, etc. And while this is not meant to instill fear or paranoia, being aware of these things helps to direct our focus for health.
These toxins can be found in the air we breathe, the water we drink, the products we use and the food that we eat. And while there are many, and I do encourage you to do more of your own research into this, let’s just pinpoint one in particular that has a major influence on gut health: glyphosate.
Glyphosate is a broad-spectrum herbicide. It is the active ingredient in Roundup, a nasty weedkiller developed by Monsanto (now owned by Bayer), and sadly, is the most widely used herbicide in the world.
Glyphosate works by inhibiting the shikimate pathway—a metabolic route found in plants, fungi, algae, and bacteria. Humans don’t possess this pathway, which is why its use was once thought "safe" for us. But the shikimate pathway is a metabolic pathway that bacteria need to make nutrients such as folate and amino acids for their growth.
So, glyphosate inhibits the shikimate pathway in bacterial cells in your gut. When this pathway is blocked, in plants, it causes death. In bacteria, it causes dysfunction, starvation, and collapse of metabolic functions. And when these beneficial microbes in our gut are dysfunctional or are dying off, this allows for the takeover of harmful bacteria.
Also, our gut microbes help us to synthesize amino acids such as tryptophan, tyrosine and phenylalanine. And if this process is not functioning, it can affect immunity, mood, sleep, focus, and hormonal and metabolic health. The metabolites produced from the shikimate pathway also support our bodies folate and methylation cycle, as well as glutathione production and metabolism.
Other harmful effects of Glyphosate:
Endocrine Disruption
Mimics estrogenic activity and interferes with hormone signaling
Liver and Kidney Damage
Shown in animal and human studies to cause cellular stress in detoxification organs
Neurotoxicity and Behavioral Effects
Linked to oxidative stress and neuroinflammation—implicated in ADHD, autism, and depression
Carcinogenicity
The World Health Organization’s IARC classified glyphosate as a “probable human carcinogen” (Group 2A)
It is a major carcinogen without doubt!
Mineral Chelation
Binds to minerals like manganese, zinc, and iron, making them unavailable to the body and to plants (which is also a major player in nutrient deficiencies in our food)
Can contribute to deficiencies and metabolic disorders
Disruption of Mitochondrial Function
Interferes with cellular respiration and energy production
Glyphosate is found in non-organic and GMO foods, especially grains, corn and soy. It is also found in water that we bath in and drink, in the air we breathe, and even alcoholic beverages and honey have tested positive for glyphosate residues. It is highly damaging to our food, our soil, our environment, and our health. And it is one of the major factors contributing to gut dysbiosis. Glyphosate has been shown to increase intestinal permeability in animal models. And it indirectly stimulates the release of zonulin by causing gut microbial dysbiosis and inflammation.
What about stress? 😫
Persistent mental and emotional stress can be a significant contributing factor towards leaky gut. When you are in high states of stress, especially for prolonged periods of time, it has some pretty dramatic impacts on your health. Too much stress can suppress the immune system. And this affects the gut microbiota in a negative way, further promoting gut dysbiosis.
High stress also affects histamine release. The compounds released when you are overly stressed stimulate more histamine to be released and affect histamine breakdown. So, what are those compounds and how can they impact gut health?
Cortisol:
In healthy levels, cortisol is an anti-inflammatory hormone, but when elevated chronically due to stress:
It weakens tight junction proteins (like occludin and claudin), causing intestinal permeability
Allows undigested proteins, toxins, and microbes to escape the gut and enter the bloodstream
Triggers an inflammatory immune response, potentially leading to autoimmunity, skin flares, or brain fog
Shifts the balance toward pro-inflammatory bacteria and decreases beneficial strains
Reduces stomach acid, leading to poor protein breakdown and bacterial overgrowth
Inhibits digestive enzymes and bile flow, which impairs fat digestion and detox
Decreases gut motility
Corticotropin-Releasing Hormone:
Directly stimulates mast cells (especially in the gut and skin) to degranulate (release chemicals from granules), releasing histamine, cytokines, and other inflammatory mediators.
Adrenaline (Epinephrine) & Noradrenaline (Norepinephrine):
Released by the adrenal glands and nervous system
These catecholamines activate mast cells and basophils (a type of white blood cell that play a role in the immune system's response to allergens and pathogens, particularly parasites)
They potentiate histamine release indirectly by sensitizing receptors and increasing tissue reactivity. And they can also promote tachycardia, flushing, and anxiety, mimicking histamine excess.
Acetylcholine:
A parasympathetic neurotransmitter found in certain tissues like the skin and respiratory tract can trigger mast cell activation
Plays a role in stress-induced urticaria (hives) and asthma-like symptoms
Substance P:
A neuropeptide released during emotional and physical stress
Stimulates mast cells and nerve endings to release histamine
Especially active in the gut, skin, and respiratory tract
Linked to pain, anxiety, and inflammatory responses
Pro-Inflammatory Cytokines (IL-1, IL-6, IL-17, TNF-α):
Produced during times of infection, chronic stress or trauma
Prime mast cells to become hyper-reactive
Alter the blood-brain barrier and influence mood and cognitive clarity
Compromise the integrity of the gut mucosal lining
Cytokines and histamine feed into each other in a feedback loop
These cytokines in particular are not meant to be a bad thing. But if they are overstimulated then they can become a problem. Inflammation is a critical process in the body’s ability to heal. But too much inflammation leads to poor health.
If you are someone who has SNPs in their genotype for any of these cytokine proteins, then stress management becomes even more crucial, as these could potentially lead to an increase in susceptibility to inflammation, infection or disease.
Here is a snapshot of my cytokine protein genes:
As you can see, managing my stress levels is something I must prioritize.
Stress compounds take up valuable resources needed for histamine breakdown and shifts the focus from ‘rest and digest’ to ‘fight or flight.’ When stress is high, the production of stomach acid is also reduced. This means there will be reduced digestion of foods and proteins such as gluten which can further damage those tight junctions and allow larger food particles to pass through. Lower stomach acid also reduces your body’s capacity to deal with pathogens and bacteria in food.
Remember earlier when I talked about how my flare ups seemed to be more prominent at night? Let’s take a look at that real quick.
Your immune system runs on a circadian clock. And at night, the balance shifts. Pro-inflammatory cytokines (like IL-6, TNF-α, and IL-1β) naturally increase in the evening and peak during times of sleep (normally between 2-4 am), and hormones such as cortisol decrease, since cortisol follows a daily rhythm that bottoms out around midnight.
Its nightly dip removes an important buffer that can keep autoimmune flares in check during the day (if the hormone is not overstimulated by stress). Cytokines are meant to be natural immune regulators. They are released to repair, clear pathogens, and regulate tissue renewal. But when elevated too much they become damaging.
They recruit immune cells to sites of injury or invasion, increase vascular permeability (to bring immune cells to the tissues), activate antimicrobial defenses, and trigger fever and tissue repair mechanisms. But in the face of chronic infection, toxin exposure, gut dysbiosis, or unresolved trauma, their signal doesn’t shut off, causing them to become even more “pro-inflammatory.”
This creates an environment where inflammatory responses can rise unchecked. And histamine, a key player in itching and skin inflammation, also peaks at night. Core body temperature also naturally increases during the second half of the night (as melatonin modulates thermoregulation). And this warmer environment can intensify itchiness and flare-ups, particularly in areas already inflamed.
Now let’s take a look at food, which can be a big deal for many people when dealing with leaky gut.
Which foods may contribute to or worsen leaky gut? 🍩
There are some foods out there that can contribute to a leaky gut. Some of the compounds within these foods can raise histamine levels and inflammation, and if you have any food intolerances or sensitivities already present, then these foods can also worsen the situation.
🥐 Gluten - this was talked about previously and this protein is primarily found in grains like wheat, barley, and rye. As mentioned before, gliadin, a component of gluten, has been shown to be a powerful trigger for zonulin release. And gluten can be particularly problematic if you already have a gluten sensitivity or celiac disease. It can cause inflammation in your gut lining, leading to increased permeability. But even if you aren’t sensitive to this food, consuming large amounts could irritate the gut over time, especially if it contains chemicals like glyphosate.
🥛 Dairy - Some researchers think that dairy contributes to leaky gut and others do not. But if the gut is already having problems, some milk proteins (especially from cow’s milk) may trigger or exacerbate autoimmune conditions in some individuals. When undigested milk proteins enter the blood stream, the immune system is triggered to generate antibodies to these proteins. And this could lead to the immune system mistakenly attacking the body's tissues, thinking it is a foreign protein. Remember earlier when I was talking about bile? If you are someone who is having gallbladder issues or if you are having problems with your bile, then consuming excess fat could be contributing to the problem.
🍧 Sugar - Some individuals are more sensitive to sugar than others. But the reason sugar can be harmful in this regard is because it can feed the harmful bacteria and fungi in your gut, creating a gut microbiome imbalance that leads to inflammation and damage to the intestinal lining. And if you are someone who is already dealing with something like candida overgrowth, sugar will further fuel that fire. Sugar can also just be a very inflammatory food for some people (I’m some people!)
🍿 Processed foods - These often contain artificial additives, like artificial sweeteners, dyes, and preservatives (all of which have their own detrimental side effects to health), as well as unhealthy fats. And many processed foods are also made with GMO products. The additives in processed food are designed to kill bacteria, to preserve it to make it last longer, to heighten the sensitivity of your tastebuds, and to make the food look more appealing. But these additives can also affect the bacteria in your gut as well as produce heightened inflammation.
🍎 Non-organic produce: Non-organic fruits and vegetables are sprayed with herbicides and pesticides that are designed to kill and deter insects, prevent the growth of harmful molds and kill unwanted “weeds”. These same chemicals will poison both you and your friendly gut bacteria. When buying conventional produce, you also run the risk of buying foods that are genetically modified.
🥩 Conventional meats - When you purchase animal foods that are not organic, grass fed, wild caught, etc., then you are buying animals that were raised through conventional farming methods. Methods that involve feeding animals lots of grains, cottonseed, canola, and alfalfa (that are all likely GMOs and high in omega 6 fatty acids) as well as the use of antibiotics in order to increase weight and yield and prevent disease due to those animals living in overcrowded conditions. And when you eat those animal foods those antibiotics and glyphosate residues are now getting into your body (antibiotic resistance anyone?). Not to mention the quality of the animal’s muscle tissue is lessened because it now holds more fat within the muscle and the profile leans heavier in omega 6 instead of omega 3, which has some pretty negatives effects of its own on your overall health.
🥤 Soda and excessive caffeine - These beverages can disrupt the gut's natural pH balance and are usually high in sugar or artificial sweeteners. These can increase gut inflammation and damage the intestinal lining. Caffeine in itself is not necessarily a bad thing to consume as it has its own benefits. But consuming it in excess can become a problem. (Did you ever see those videos of the guy cleaning the chrome of his truck with Coca-Cola? Or what about the guy who cleaned his toilet with it? Gross! Definitely not something I would want in my stomach!)
🍷 Alcohol - These drinks can be particularly harmful and contribute to a leaky gut in a number of ways. Firstly, alcohol is naturally high in histamine. It also promotes candida overgrowth by suppressing your immune system and changing your microbiome by feeding it excess sugars. When alcohol is broken down, a toxic byproduct called acetaldehyde is formed. And acetaldehyde can further damage the tight junctions between your gut cells. (Don’t freak out though! This is something that I’ll come back to when I get to part 2).
🌶️Night shades - People who are already dealing with leaky gut or some sort of autoimmune condition like IBS, psoriasis, or rheumatoid arthritis will likely have sensitivities to these types of foods. Nightshades include foods and herbs like tomatoes, peppers, white potatoes, goji berries, eggplant, ground cherries, ashwagandha and tobacco. These foods contain compounds called solanine and tomatine. These compounds can bind to cholesterol in cell membranes, and which could increase intestinal permeability, increase inflammation and produce cytokine release.
Now that we have looked at some of the major causes or contributing factors to leaky gut, let’s move on to part two.
Part Two: The How 🌟
The Pathway to Healing:
The pathway to healing begins with the understanding of information. Once the causes and mechanisms are understood you can then use that knowledge to guide you. I will tell you that this has not been an easy journey for me, and I can assume that if you are dealing with this too, it has not been an easy one for you either. The good news is that there are certain steps and lifestyle changes that can be made to improve your health and heal your gut.
The key factors to focus on here when you are beginning is to establish lifestyle choices and habits that you feel good about and that you can sustain long term. Even before beginning any sort of supplement routine or health hack, you should always start with the basics first. We are going to take a look at what it really means to cover the basics. Then we are going to look at some other helpful tools like types of testing you can take and what kinds of supplements may potentially be beneficial for you.
But of course, make sure to always consult with your healthcare provider if you are already seeing one. You want to make sure that you are ruling out or possibly taking care of other possible health issues before jumping into this. Just remember, mastering the basics is crucial to optimal and long-term health!
Diet: 🍽️
This has been a huge contributing factor in my own path to healing. Over the years I have experimented with so many styles of eating. I was vegan for about 2 years, and 100% raw vegan for about 6 months of that time. I’ve done vegan keto, normal keto (clean version), the carnivore diet, the paleo diet, the AIP protocol diet, and the Mediterranean diet. And after all of that, the best advice that I can give to you is to tell you this:
Everybody is different. Every individual is going to fare better with different foods. And diet is not a one size fits all. You have to find the style of eating that is best for you and your own circumstances. You have to decide for yourself what you are and are not willing to consume based upon how you feel. Stop chasing every fad diet out there and listen to your own body!
With that being said, you want to make sure that you are doing your best to eat a healthy diet, whatever that looks like for you. But a good general consensus is to stick to whole foods. When it comes to leaky gut, it is a good idea to start with an elimination style diet.
And this is not actually a form of diet, but rather a way to discover what foods you can and cannot tolerate. Cut out any foods, spices or drinks that are nightshades and that are high in histamine. Give it at least one to two weeks and then slowly add back in one food at a time, watching for any symptoms over the following 1-3 days. They may show up withing a few minutes or a few hours, or it may take several days. And keeping a food journal during this time can be a really helpful tool.
High histamine foods:
Aged cheeses
Tomatoes
Citrus fruits
Eggs
Legumes
Dried fruits
Eggplant
Pineapple
Papaya
Chocolate
Shellfish
Fermented foods
Cherries
Peanuts
Spinach
Cured meats
Bone broth
Vinegars
Alcohol
For me personally, after doing this I discovered that I absolutely cannot tolerate eating tomatoes. I can eat peppers occasionally, but not too much (though bell peppers don’t seem to bother me at all). I also noticed that the hotter the pepper, the worse my reaction was. And eating too many oranges or too much dairy does not fare well for me either.
Sugar and grains also cause some major issues for me. I also noticed that I would have symptoms show up a few days after consuming alcohol, especially wine. But I would also get a lot of ear and facial flushing while I was drinking. During those days following adding foods back in, you will want to watch for symptoms like:
Digestive issues (pain, cramping, bloating, bowl movement issues, etc.)
Respiratory symptoms (congestion, runny nose, sneezing, etc.)
Skin flare ups (acne, rashes, hives, etc.)
Achey or stiff joints
Flushing of heat and redness in the ears and face
Headaches or migraines
Fatigue
Anxiety
Heart palpitations
Basically, all of the same symptoms listed earlier when talking about histamine
If you notice any symptoms like these after consuming any reintroduced foods, then you know that those foods need to be eliminated from your diet or at least limited quite a bit. Cutting back on the amount of dairy you consume could also help. You might also want to consider trying out different forms of dairy, like goat milk or cheeses, or even camel milk if you can get it. As those types of dairies usually work much better for people who have gut issues or who have lactose intolerance. A little bit of heavy cream in your coffee or a tiny bit of cheese here and there might not be a big deal. But again, just pay attention to how your body reacts.
Sugar is something that really should be completely eliminated from the diet if possible. Especially if you are dealing with something like candida. And when I say sugar, I mean processed sugar and drinks like soda. In the beginning it may also be wise to either limit your fruit intake or eat fruits that are lower on the glycemic index like berries, and switch your coffee or tea sweetener to honey, stevia, or monkfruit in smaller amounts until you feel like your gut has healed. Once you are beginning to feel better, you can always add in more fruit and see how your body handles it.
When it comes to gluten, if you know or think you may be dealing with leaky gut, or if you have an autoimmune condition, you need to get rid of anything made with wheat, barley or rye. Not only will you be getting rid of the gliadin proteins, but you will also be lowering any potential of consuming GMOs or grains with glyphosate residue. If you wish to try to add back in a slice of bread or a side of pasta here and there, then try to opt for organic products to help reduce any negative effects. And I would wait to do this until you feel that you have become more stabilized with your health.
When it comes to buying organic foods, do what you can. Not everyone can afford to buy all of their fruits and vegetables organic. And the same goes for grass fed meat and wild caught fish. And not everyone has access to a wide variety of these foods. But when you have the options available and the means to do so, go for it. At a minimum, you could also opt out of buying conventional for the “dirty dozen.” This list is for foods that are going to contain the highest amount of pesticide residue and are the ones that should definitely be avoided if possible.
Dirty Dozen:
Apples
Strawberries
Spinach
Kale
Collard greens
Mustard greens
Grapes
Peaches
Nectarines
Peppers
Cherries
Blueberries
Green beans
Some good styles of eating you might want to consider trying out are the paleo diet, the Mediterranean diet (minus any nightshades that affect you), or the AIP (autoimmune protocol) diet. All of which I have tried, like I mentioned before. But remember, this isn’t about sticking strictly to “fad diets,” this is just about finding what foods work best for you.
My current style of eating is a bit of a combination of all of those. I shoot for a higher amount of protein (1g per lb of body weight), good healthy fats in moderate quantities, moderate to low carbohydrates (from fruits and vegetables), no processed sugar, no nightshades, and no grains (though I will have a bit of rice occasionally). I cook my food with butter, bacon grease, tallow, avocado oil or coconut oil. And I alternate between higher and lower glycemic fruits and vegetables depending on where I am in my menstrual cycle. But as I said before, your diet needs to be tailored specifically to you.
And while we are on the topic of food, let’s talk about another related topic, chewing your food. I know this may seem like a silly thing, but it actually is important that you are making sure to properly chew up your food before swallowing it. So many of us just inhale our food instead of taking the time to really break it down in the mouth. But believe it or not, this can actually be contributing to your issues with leaky gut.
When you properly chew your food, you make it easier for your stomach acid, enzymes, and bile to break it down even further. This helps to prevent large, undigested particles from reaching the small intestine (which can trigger inflammation or immune responses). Your saliva contains enzymes, electrolytes and bicarbonate.
Enzymes like amylase and lipase help with carbohydrate and fat digestion. And the latter two (electrolytes and bicarbonate) help with pH balance and protecting the mucosa. And the more you chew your food, the more saliva you produce. Chewing slowly and consciously also stimulates the vagus nerve which can help to shift you out of heightened fight or flight response.
One last note on diet:
Something interesting that I discovered recently was that eating leftovers could also be contributing to leaky gut. Leftovers!? But most of us eat leftovers, don’t we? Yes, we do. It is so much easier to keep up with our fast-paced modern lifestyle when we can meal prep and have our food ready to go for the week to take with us to work or school. It can help to keep us on track with a healthy whole food diet when we are able to cook at home and have good meals already prepared.
I think we all know that older food can produce bacteria. But I think that most of us think of this in the way of toxic bacteria that can make us sick. You won’t eat food that got left out on the counter overnight. And you won’t eat food after it has been sitting in the fridge for 5-7 days. But here is the interesting thing, the downside to this is that leftovers actually have histamine producing bacteria. Even the very next day after being in the fridge they start to grow. And the more days they sit, the more of these bacteria will be present in the food.
So, if you are someone who is struggling with leaky gut, autoimmune disorders, impaired DAO enzyme function, histamine intolerance, etc., then limiting the amount of leftovers you eat is going to help. I have personally started not to eat any leftovers passed two days. I make enough food for that day and the following day for lunch and dinner. If I decide to make a big batch of something, I will separate it out into individual portions and put it in the freezer, because freezing those leftovers inhibits the growth of those bacteria. That way I can take out a portion to be eaten only on that day.
Sleep: 💤
Getting deep restorative sleep is crucial for health; critical metabolic processes, hormone regulation and detoxification all happen when you are asleep. When you are sleep deprived it can wreck your day and even have lasting effects for several days after. It also raises your cortisol levels which can increase intestinal permeability.
But why is good sleep so important for gut health?
Because when you are getting sufficient amounts of sleep, your body regulates the immune system. It reduces inflammatory cytokines like IL-6 and TNF-α (unless you are overly stressed, have heavy toxic burden, are already dealing with strong inflammation, or are dealing with an infection), increases regenerative cytokines like IL-10, activates T regulatory cells which calms autoimmune responses, and your GALT (gut-associated lymphoid tissue) shifts into repair mode.
Good sleep also helps maintain microbial diversity and balance. It stimulates intestinal epithelial cell turnover, upregulates genes involved in barrier repair, and you get a release of melatonin which has antioxidant and gut-healing effects.
If you are someone who is not getting good quality sleep because of insomnia or because you keep getting woken up from high histamine symptoms, then this is something that will need to gradually be regulated over time. If you are struggling with sleep, melatonin can be good to try out, as that is a fairy common supplement today. But another thing that may help you that is not as common is glycine, a non-essential amino acid and inhibitory neurotransmitter that works alongside GABA. But once you are able to establish the other basics, and perhaps after other measures like supplementation are taken, you will be able to sleep more soundly.
Exercise: 💪
I think we all know how good exercise is for maintaining good health. And I am a big proponent of building healthy lean muscle for longevity. But ultimately, you want to find an exercise routine that will work best for you. Making sure that routine fits into your schedule without creating excess fatigue and making sure it is a style of exercise that you actually enjoy are important factors in ensuring that you can sustain it long term. As long as you are moving your body in some way you are on the right track.
But how exactly can exercise be beneficial to gut health?
Regular movement increases the diversity and quantity of gut microbiota—especially beneficial strains like:
Akkermansia muciniphila – supports mucosal barrier integrity
Faecalibacterium prausnitzii – anti-inflammatory butyrate producer
Bifidobacteria and Lactobacillus – support digestion, immunity, and mood
Exercise aids in colon cleansing and enhances lymphatic circulation which in turn enhances your immune system and helps prevent the growth of harmful bacteria. Exercise also lowers systemic inflammation and reduces oxidative stress, which helps protect gut lining cells, and increases butyrate production, which fuels colonocytes and tightens the junctions of the gut wall.
Reducing Toxic Exposure: 🚫
It can be hard to get away from many of the toxins in our environment. But trying to eliminate or avoid them the best that you can will not only help to heal your gut, it will also help with your overall health. Do what you can to clean up your water and your indoor air quality by buying filters for your drinking water, shower and bath water.
If you have the means, buying a whole home reverse osmosis system would also be incredibly beneficial. Just make sure not to drink that water unless you are adding back in the proper trace minerals. Adding good quality air purifiers into your home will also be a good thing, especially if you spend a lot of time indoors. But if you cannot afford to go that route, just ensure that you have high quality A/C filters in your home.
If you are a home gardener, avoid the use of chemical herbicides and pesticides and go for natural products to help with molds and “weeds” or other means of naturally repelling pests like the use of copper rods or companion planting. And do what you can to offset any negative impacts from home use cleaning and toiletry products, either by buying products marketed as clean or by making them yourself.
So many of our products contain chemicals that are detrimental to our health. They create hormone dysfunction, rise our histamine levels, and create a cascade of inflammation. Everyday products like dish detergent, hand soap, laundry soap, shampoo, conditioner, body soap, hair styling products and makeup leave us overly exposed to a heavy toxic load. So, cleaning this up as much as you can will go a long way. And now there are many websites and apps out there that you can use to help you sort through the potential toxins found in the products that you use.
Sunshine: ☀️
Make sure that you are getting a good daily dose of sunshine. Modern living has definitely made it a lot harder to get adequate amounts of sun. Many people spend the majority of their day indoors while they are at work. Or perhaps even at home on days off. But getting enough sun, without burning of course, is important for healthy immune function, among many other things.
Of course, vitamin D is the key nutrient of focus here (although the effects of the different spectrums of light, like red light, have their own unique benefits to health). Vitamin D directly supports the integrity of the intestinal wall by upregulating tight junction proteins such as claudin, occludin, and zonula occludens and reduces intestinal permeability. And it promotes microbial diversity and encourages the growth of beneficial species.
Vitamin D receptors are present throughout the gut lining, especially in immune cells of the gut-associated lymphoid tissue (GALT). It regulates T cell activity which calms autoimmune responses. And it reduces Th17-mediated inflammation, which is involved in many gut disorders, including Crohn’s disease and ulcerative colitis.
And it helps increase serotonin production in the gut which helps regulate mood and stress response. But if you are someone who cannot seem to find enough time to get the right amount of sun due to work or other reasons, then getting vitamin D through a good quality supplement, as well as eating foods high in vitamin D like fish, eggs, yogurt, liver or mushrooms is a good idea.
Stress management: 🌙
Stress management is incredibly important when it comes to good health. Though our modern world can definitely make that difficult at times. There are many things that you can do to help regulate your stress and calm your nervous system. They key is finding what works best for you, your lifestyle and your schedule and put those chosen practices into a routine that you can sustain long term.
Some modalities to consider to help alleviate stress:
Meditation
Taking a walk in nature
Grounding
Breathing exercises (especially deep diaphragmatic breathing)
Yoga
Massage
Other nervous system regulators like cold plunging, polyvagal therapy, humming or chanting, or using a vagus nerve stimulator
EFT tapping
Therapy
Using adaptogenic herbs like Rhodiola Rosea, Holy Basil (Tulsi), Eleuthero (Siberian Ginseng) or Ashwagandha
Practices like Qi Gong or Tai Chi, somatic shaking, yoga nidra or dance
Drinking a calming tea like lavender, chamomile, or a nighttime tea blend
Journaling
Learning to say no without guilt and setting proper boundaries
What comes next?
After you get the basics under control, and you become wiser at listening to your body, this would be the time to take stock of any other symptoms you are still having. This would also be a good time to look into any means of testing to deepen your understanding of your own body. With any kind of medical testing, you absolutely can jump straight into this while you are in the process of nailing down your basics.
The reason I recommend waiting for this is because there may be many processes within your body that become regulated after mastering the things mentioned above. And if you are testing beforehand, that might give you more incentive to jump into other forms of correction before you have had a chance to balance out through things like diet, sleep and stress management. But if you are someone who can recognize the importance of the basics, then tackling everything at once may not be a bad idea.
So, what are some good things to test for when it comes to leaky gut?
Genetic Testing:
The sciences of genetics and epigenetics are fascinating and are producing some very valuable information when it comes to health.
Getting a genetic test done can help you to see where you could potentially be having issues (as you can see from the photos I put in of some of my own genes). It can help to give you some of the missing pieces to the puzzle.
Understand though, that just because you get a report back that shows you to have certain SNPs, that does not necessarily mean you need to go all in and act on “fixing” it. Our bodies our amazing and they work tirelessly day in and day out to maintain a state of homeostasis. You very well may have other SNPs present that are there to help offset the effects of others. And your own daily lifestyle habits play a major role in whether or not certain genes are expressed. This is why it is important to use this report along with other types of testing and with your own list of symptoms.
There are many genetic tests out there. They can either be ordered online for you to do in the comfort of your home, or they can be ordered by your health professional.
The two I would recommend choosing from would be The Works from MaxGen Labs or the StrateGene Report from Seeking Health. The first one is much pricier than the second. So just keep that in mind. Either way, if genetic testing is something that you think could help, use whatever test you find to be the most appropriate for you.
If genetic testing is something out of your reach or something you wish not to do, then you could still find resolve without doing it. You can still rely on other forms of testing to help give you answers. And you can, most importantly, listen to your body when trying out different things and simply monitor how you feel and how your health is progressing.
Gut Testing:
Gut testing can be done through the use of breath, urine and stool.
A gut health test is designed to assess the condition, composition, and function of your digestive system, bile and bile acids, as well as the microbiome.
A gut health test can be used to detect dysbiosis, assess how well your body is breaking down and absorbing food, and whether your gut lining is intact or compromised, identify inflammatory conditions, autoimmune activity, or hidden food sensitivities impacting gut health, and discover toxic internal terrain, over-fermentation, or hormone recirculation affecting the liver and gut axis.
Some tests that I would recommend for this would be the GI Effects test from Genova Diagnostics or the Gut Zoomer test from Vibrant Wellness. Again, there are many of these tests out there, and just like the genetic test they can be ordered by you online to be done at home or ordered through a medical professional. So, choose the route that is best for you.
Types of gut tests:
Comprehensive Stool Test (e.g., GI-MAP, Genova GI Effects, Doctor’s Data)
Microbiome Sequencing Test (e.g., Viome, Ombre)
Zonulin Blood/Stool Test
Organic Acids Test (OAT)
SIBO Breath Test
Intestinal Permeability Test
Sugar Testing:
Lactulose and mannitol urine test
This is another test that can help provide information about the intestinal lining and whether or not there is increased intestinal permeability.
You would consume a drink that contains these sugars and then you would provide a urine sample.
The sample would be tested to evaluate the ratio between the two. If you have more lactulose than mannitol, then that might be a sign that you are dealing with leaky gut, as lactulose is a larger molecule than mannitol.
Food Sensitivity Testing:
Leaky gut causes immune exposure to undigested proteins. This type of testing could be good to see how your body is responding certain foods.
You could use this test to check for sensitivities to gluten, dairy, nightshades, or foods that are high in histamine.
This reveals what could be provoking the immune system through a compromised barrier.
I do not have any particular recommendations for this type of testing. As I had this test done within the first year of my symptoms showing up through the office of an Allergist. But again, these can be ordered online or through your physician.
I also do not necessarily recommend this test as the best means of finding answers. It can be helpful when it comes to knowing which foods might be causing you problems. But it is not a solid answer as to why. You will still have to do a bit of guessing and playing around. It can help point you in the right direction if it really something you wish to do, and perhaps if you are leery of doing a genetic test. Because if you have a big list of foods pop up like I did, it will likely point you to two things, one: that you have a problem with histamine and therefore likely with the DAO enzyme, or two: that you have a problem with leaky gut and all of the foods that are showing up on your panel are there because they are leaking through your gut lining and making their way into your bloodstream and your body has now created antibodies for them.
Vitamin/Mineral Testing:
It is always a good idea to have your vitamins and minerals tested at least once a year.
If you are limited on the tests that you can do, checking your B vitamins, vitamin D, vitamin C, and your electrolytes is a good place to start.
This is usually done through a blood sample and can be attained through your physician or through any lab that does not require an ordered lab from a doctor.
Hormone testing:
The best test that I can recommend for this is going to be the Dutch test, which is done through a urine sample. This test is going to look all of your hormones, as well as their metabolites and it is going to give you a very good overall consensus of what your hormones are doing.
Of course, if you are only looking to check specific hormones, then there are other labs that you can do to give you a more isolated view of things.
Mycotoxin / Mold Testing:
Mycotoxins directly damage the gut lining. They directly weaken tight junction proteins (e.g., occludin, claudins, zonulin regulators), allowing intestinal permeability to rise.
Mold toxins alter the gut terrain by killing beneficial bacteria and promoting the overgrowth of certain pathogenic bacteria and candida.
Mycotoxins increase pro-inflammatory cytokines, suppress immune surveillance in some areas while triggering autoimmunity in others, and cross the blood-gut and blood-brain barriers, causing widespread effects.
The liver and bile are primary routes of mycotoxin elimination. But mold impairs Phase I and Phase II liver detox enzymes, thickens or blocks bile, and recirculates toxins through the gut, increasing reabsorption (especially if leaky).
Mold also increases anxiety, depression, fatigue, and brain fog and triggers HPA axis dysregulation, contributing to cortisol imbalances that worsen leaky gut.
I have personally dealt with toxic black mold exposure, and I can tell you that if you live in a climate that is susceptible to mold, or if you suspect that your home or place of work or school could have a problem with mold, then this form of testing would be very beneficial to you. And if this turned out to be a problem for you then you would have the knowledge you needed to take necessary action to either move or clean up your environment. Mold can be a very serious thing, and I do not take it lightly.
For me personally, finding a physician that could do the proper testing for this was a bit of a challenge. Many of the doctors I went to or called told me that they only tested for common environmental molds, not the more toxic molds like Stachybotrys Chartarum (black mold), Aspergillus, Penicillium, Fusarium, and Chaetomium. Because of this I chose to order my test online. Typically, the way this works is they send you the test kit and you take the kit to a local phlebotomist who draws the blood and sends your kit back to the company. The test that I used was the Myctotoxin test through MyMycoLab. But of course, use whatever test you think is best.
Heavy Metals Testing:
Heavy metals can be tested by blood, urine or hair samples.
Vibrant Wellness and Genova Diagnostics also offer heavy metal testing. But there are many you can choose from.
Heavy metals like mercury, arsenic, cadmium, and lead can destabilize gut flora, weaken immune regulation, erode the epithelial lining, and prevent your detox pathways from functioning as they should. They can also have really detrimental effects to cellular health and brain health.
If you discover that you have a toxic overload from either mold, heavy metals or both, then there are things that you can do to help your body get rid of them. Detox protocol is not something that I am going to cover here, but I will likely talk about that in a future article. But you can either do your own research or get in touch with a knowledgeable health professional so that they can help you through the process.
Let’s Talk Supplements:
When it comes to nutrients like macros, vitamins and minerals, something to understand is that the RDI or RDA requirements are only there to prevent deficiency, not to optimize health. They were put in place to prevent people from getting things like scurvy, rickets, and pellagra. There is a rather interesting story behind this, but it is not one that I will go over here. Though it might be something worth looking into on your own time if it interests you.
When it comes to leaky gut, and any associated issues like autoimmune conditions or histamine intolerance, there are some supplements out there that could be beneficial for you. But understand that the supplements are not meant to be your crutch. They are simply a tool in your toolbox that can give you that extra boost if it is needed. Maintaining a healthy diet and healthy lifestyle choices should always be number one. You can’t make poor choices and expect to supplement your way out of it. That will not work in the long term.
A quick note on antihistamines before moving onto supplements:
Some people may logically think that antihistamines are going to help. And coming from experience, yes, they can, but only short term. Antihistamines are not something that you want to have to continue to lean on. Different antihistamines work in different ways. Some of the more common drugs like Zyrtec and Benadryl (both of which I used to use on a regular basis) work by blocking the histamine receptors, making histamine unable to bind.
This can be a good thing if you are experiencing very severe symptoms. The problem is that all of that histamine is still floating around in your system. And once the antihistamine is gone, those receptors become available and all of that histamine goes rushing back in, bringing all of the symptoms back. This is why I was having to take those drugs every day and night to get lasting relief. But it wasn’t solving the problem.
And long-term antihistamine use can come with some unwanted effects. Things like impaired memory and learning (by blocking acetylcholine), increased risk of dementia, interference with sleep, reduced connection to bodily cues, and immune dysregulation. And long-term use can also contribute to dysbiosis in the gut microbiome.
What are some good supplements to consider?
Probiotics:
The genus Lactobacillus includes dozens of species and hundreds of strains, each with unique effects on the immune system, histamine levels, and gut barrier integrity. Some strains are immunomodulating and anti-inflammatory. Others are histamine-producing or pro-inflammatory. For someone in a state of immune excess, certain Lactobacillus strains are histamine producing strains and some can amplify inflammation. Strains to watch out for:
Lactobacillus casei
Lactobacillus bulgaricus
Lactobacillus helveticus
Streptococcus thermophilus (often paired with them in yogurts)
Many Lactobacillus strains produce L-lactic acid, which can lower pH (beneficial in small amounts, but damaging in excess), feed certain pathogenic bacteria or fungi and irritate sensitive gut linings.
In people with:
Low bile flow
SIBO (small intestinal bacterial overgrowth)
Chronic fatigue, fibromyalgia, or MTHFR mutations
This lactic acid buildup can contribute to:
Bloating, fatigue, brain fog, and acidosis-like symptoms
Some Lactobacillus strains can also displace more beneficial strains like Bifidobacterium.
Some beneficial strains that do not produce histamine and strengthen the intestinal lining:
Bifidobacterium infantis
Bifidobacterium bifidum
Bifidobacterium longum
Bifidobacterium lactis
Ligillactobacillus salivarius
Lactiplantibacillus plantarum
Bifidobacterium breve
Lactobacillus rhamnosus GG
Lactobacillus plantarum
Lactobacillus salivarius
Bacillus coagulans
Bacillus subtilis
Saccharomyces boulardii (Not a bacteria but a non-colonizing probiotic yeast that supports gut lining repair and inhibits harmful bacteria)
B-vitamins:
Vitamin B6 is one of the cofactors for making DAO and also plays a major role in the methylation pathways. It also supports serotonin and dopamine balance, which can often be disrupted by histamine overload.
B9 and B12 provide the body with methylation support, and they clear histamine through the COMT and HNMT pathways.
These B vitamins are crucial components in all of the methylation pathways in your body. But always be cautious with them, especially if you have discovered through genetic testing that you have any SNPs that affect your methylation. The topic of methylation is a deep rabbit hole and one that I will likely cover sometime in the future. But just know that taking the wrong form of these vitamins or taking them in excess can also have some negative effects. But you will likely need to avoid the forms marketed as folic acid and cyanocobalamin. And depending on your own personal health, you may need to take other forms like folate (5 methyltetrahydrofolate), folinic acid, methylcobalamin, hydroxocobalamin, or adenosylcobalamin. So as always, be sure you are listening to your body and if needed working with a health care professional to help with this.
Vitamin D:
As I talked about earlier, if you are someone is not getting ample amounts of daily sunshine, then taking a good vitamin D supplement may be beneficial for you. Just be cautious with it if you are already taking a calcium supplement, because vitamin D increases intestinal absorption of calcium. Calcium may accumulate in the soft tissues, including arteries, kidneys, and joints which can lead to calcification, kidney stones, or inflammation. Vitamin K2 can also be a good thing to take with vitamin D because together they can improve outcomes in osteoporosis, heart disease, and autoimmunity more than either can alone. Vitamin K2 also helps to guide calcium to the bones and not the arteries.
Vitamin C:
Not only is it great for immune system regulation, but it is also beneficial for healing leaky gut.
Vitamin C is essential for maintaining tight junctions and can help to heal ulcers, erosions, and microtears in the gut wall.
It scavenges reactive oxygen species, inhibits NF-κB, the master gene of inflammation, decreases cytokines like TNF-α and IL-6 and quiets overactive mast cells and histamine release.
70–80% of the immune system resides in the gut-associated lymphoid tissue (GALT), and vitamin C helps to keep the immune system strong and functioning properly. It enhances IgA production, your gut’s protective antibodies, increases phagocyte activity (clearing of pathogens), supports T-cell function without triggering autoimmunity and protects against viral, bacterial, and fungal invaders.
Vitamin C can also bind toxins and enhance glutathione recycling, protect the liver from oxidative stress and reduce ammonia, mold, and heavy metal burden.
Electrolytes:
Electrolytes, especially magnesium and potassium, are critical for coordinating smooth muscle contractions, preventing constipation or diarrhea, and supporting the nervous system.
They help to reduce cytokine production, buffer oxidative stress, and support adrenal function.
Electrolytes support the tight junctions between intestinal cells.
Magnesium also supports zonulin modulation.
Sodium and chloride regulate water movement in the gut lining.
Proper electrolyte levels maintain ideal pH for beneficial bacteria, prevent overgrowth of pathogens (which thrive in acidic, imbalanced terrain), and enhance production of short-chain fatty acids like butyrate.
In any gut imbalance that causes fluid loss (IBS, SIBO, food poisoning, stomach bugs), electrolytes are rapidly depleted. Replenishing them prevents dehydration, restores cellular integrity, and supports immune defense in the gut wall.
Digestive enzymes:
These are proteins that break down food into its absorbable components.
Some enzymes are produced in the saliva. Some are produced in the stomach or the small intestine. And others are produced in the pancreas.
Digestive enzymes ensure maximal nutrient absorption of amino acids (to rebuild gut lining), fatty acids (to reduce inflammation), and vitamins and minerals (to support repair and detox).
If you are someone who struggles to chew your food properly, or if you are having issues with breaking down certain foods, then these could be beneficial for you.
Enzymes restore the flow of digestion, minimizing fermentation and easing pressure on an already fragile lining.
Certain enzymes like DPP-IV can help to neutralize inflammatory peptides. And proteolytic enzymes like serrapeptase or bromelain can also be taken between meals to reduce systemic inflammation.
Lactase can help break down lactose for those with dairy sensitivity. And interestingly enough, when dairy products are processed, this naturally occurring enzyme is removed. Lactase is needed to break down lactose. This is why many people who think they are lactose intolerant actually find that they do much better with raw dairy, because the lactase is still intact.
Ox bile or lipase can help with fat digestion (especially if gallbladder is compromised).
Some cautions:
People with ulcers or gastritis may need to avoid acidic enzyme blends at first.
If SIBO is present, high-fiber diets plus enzymes may worsen symptoms temporarily.
DAO enzyme:
If you are struggling with a DAO gene that is not functioning properly, or if your DAO enzyme is hindered in some way by any of the things talked about previously, then this could be a good supplement to help support those enzyme levels and help to tackle elevated histamine
You could also take this if you knew that you were going to be consuming high histamine foods or alcohol to help offset any potential symptoms. This is not something you want to do all the time though. You still want to clean up your diet for long term health.
Quercetin:
Inhibits mast cell degranulation, downregulates histidine decarboxylase, the enzyme that produces histamine, and calms allergic responses in the gut lining.
A modulator of immune responses and a free radical scavenger.
Enhances the expression of occludin and claudin, key tight junction proteins, and promotes gut epithelial regeneration.
Has broad-spectrum antimicrobial activity.
Enhances phase II liver detox enzymes, increases glutathione levels and improves bile secretion.
The bad news is that quercetin is a methylation inhibitor and can be particularly problematic for people with COMT V158M (slow COMT), MTHFR mutations, or histamine SNPs like DAO, HNMT. If you deal with any of these things then it may cause irritability, fatigue, or anxiety. It could also aggravate histamine symptoms and worsen the body’s ability to detox.
Zinc L-Carnosine:
A chelated compound where zinc is bound to L-carnosine in a 1:1 ratio.
Zinc is essential for cell regeneration of the gut lining cells, tight junction integrity, and wound healing at a cellular level. And carnosine enhances cellular resistance to oxidative stress, mitochondrial function in epithelial cells and peptide signaling for tissue repair. But together they help to rebuild the gut wall, increase mucin secretion and strengthen the tight junctions, reducing permeability. And taking it in this form is more beneficial than taking them separately.
Methylsulfonylmethane (MSM):
Delivers bioavailable sulfur which is essential for structural proteins like collagen, elastin, and keratin.
Known for its anti-inflammatory, detoxifying, and tissue-rebuilding properties.
Reducing levels of pro-inflammatory cytokines and decreases mast cell degranulation and histamine release.
Increases glutathione levels.
Supports Phase II liver detoxification.
Assists in the removal of xenobiotics and inflammatory byproducts.
Take caution if you are on any anticoagulant medications because it may thin the blood slightly.
Sulfur-sensitive individuals or those that have any SNPs in the CBS gene (which is also something that I have in my genetic profile) should also take caution and ensure that you go slowly with low doses.
N-Acetyl D-Glucosamine (GlcNAc):
A precursor to glycosaminoglycans (GAGs)—compounds essential to mucus production, gut wall structure, and immune signaling.
Found in the mucosal lining of the GI tract, synovial fluid, and cartilage.
Rebuilds the gut mucosal barrier.
Reduces inflammatory autoimmune activity.
Helps stimulate the production of mucin which provides moisture and protection.
It has also been shown to reduce neuroinflammation an improve myelin repair, which can help with brain fog, anxiety, depression, or neurological immune disorders like MS.
Because the gut, skin, and joints all rely on glycosaminoglycan structures, it can help to improve collagen matrix integrity, relieve eczema, psoriasis, and other leaky gut-associated skin issues, and aid in joint fluid production and repair.
Many sources are shellfish-derived, so please avoid this if you have a shellfish allergy or find one that is from a different source.
Overall, this supplement is known not to spike blood sugar even though it is a glucose derivative. But it may raise insulin sensitivity slightly, so just be sure to monitor your blood sugar if you are diabetic.
Best used alongside mucilaginous herbs.
Herbal supplements:
Licorice root:
Make sure it is deglycyrrhizinated (DGL).
Promotes mucus production and healing of the gut lining.
Has anti-inflammatory and anti-ulcerative effects.
Cat’s claw:
Reduces inflammatory cytokines and balances Th1/Th2 cytokine expression.
Support tight junction repair.
Promote tissue regeneration, especially in the intestinal epithelium.
Inhibits overgrowth of yeast, bacteria, and viruses.
Contains polyphenols that help to neutralize free radicals and protect the gut from oxidative damage.
Stinging nettle:
Soothes systemic and localized inflammation in the gut wall.
Helps rebuild the intestinal wall and tighten loose junctions.
Inhibits histidine decarboxylase, an enzyme that produces histamine.
Stimulates lymphatic flow and encourages urinary detoxification.
Nourishes the adrenals.
Slippery elm bark:
Mucilaginous herb that coats the gut lining with a protective barrier.
Reduces inflammation and encourages tissue repair.
I have personally been using this herb from the beginning and it is always the first one I recommend.
Marshmallow root:
Mucilaginous herb that softens and moistens dry, irritated tissues.
Has been known to soothe ulcers, heartburn, IBS, and gut inflammation.
Supports the regeneration of intestinal epithelial cells.
Milk thistle:
Supports phase I and phase II detoxification, helping the liver process histamine, mycotoxins, endotoxins (from leaky gut or bacterial die-off) and environmental toxins.
Reduces intestinal inflammation triggered by gut permeability.
Protects gut lining cells from oxidative stress.
Supports the healing of ulcers and inflamed mucosa.
Enhances bile production and quality.
Has been shown to inhibit mast cell degranulation, reduce histamine release and calm cytokine storms associated with allergies, eczema, asthma, and leaky gut.
Calendula:
It is anti-inflammatory and antimicrobial.
It is also an astringent which helps to tighten loose junctions.
Helps to speed up epithelial tissue repair.
Turmeric (curcumin):
Anti-inflammatory and antioxidant.
Supports liver detox (aiding gut-liver axis).
Enhances tight junction expression and mucosal repair.
This is also one that I have used a great deal to help calm the storms of inflammation.
Aloe Vera:
The inner leaf gel can help to soothe inflamed tissues.
Encourages collagen repair of the gut lining.
It is also antimicrobial.
Ginger:
Stimulates digestion and reduces bloating and nausea.
Enhances motility which can help with SIBO and stagnation issues.
Anti-inflammatory and supports immune modulation.
If you made it to the end of this that is amazing! I know this was a lot of information. I just want to say a huge thank you for reading my content. And I also want to say that I am so very proud of you for wanting to take back control of your health and heal your body. That is a huge deal, so get excited! 😄
Your gut is a powerhouse to health. It is your own inner sun. You have to nourish it so that it can remain bright and radiant and keep you living a long and healthy life. If you don’t, you can become lost in the dark with illness and disease as your company. And speaking from experience, this is not an easy place to be.
I hope that in reading this you have gained the knowledge that you need to heal and thrive, as that was my goal in doing this. I hope that you choose to take this information and place it into your own toolbox, continue to do your own research, and reach out to the necessary people who will continue to help you on your journey. Many blessings. 💚







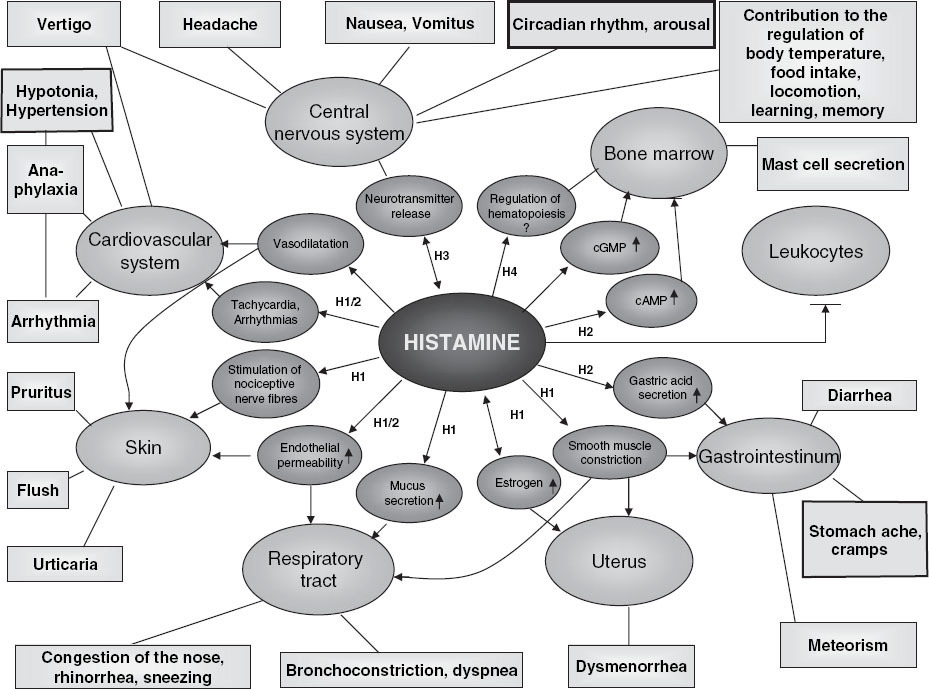

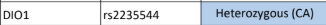
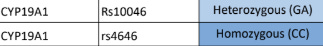

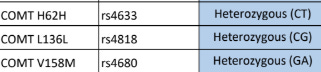

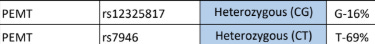


Thank you Summer! Very informative and tons of actual solutions 💜